
Venous Stasis Ulcers
Venous stasis ulcers are painful, slow-healing sores on the leg that occur from backwards blood flow in the veins of the limb. They typically occur on the lower part of the leg at or above the onside of the ankle when blood pools and can’t pump back to the heart, a condition known as chronic venous insufficiency.
In some cases, venous stasis ulcers can lead to serious complications, such as necrosis or severe ulceration. Fortunately, there are treatments for venous insufficiency that can prevent the future development of venous ulcers.
Venous Insufficiency and Venous Ulcers
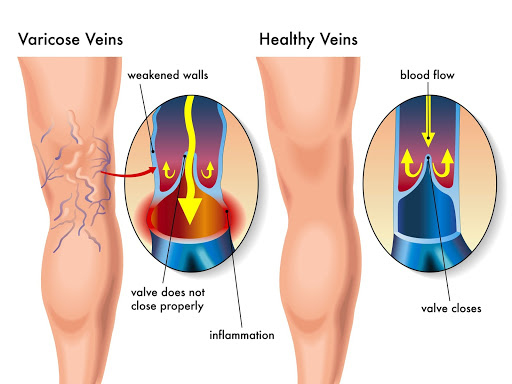
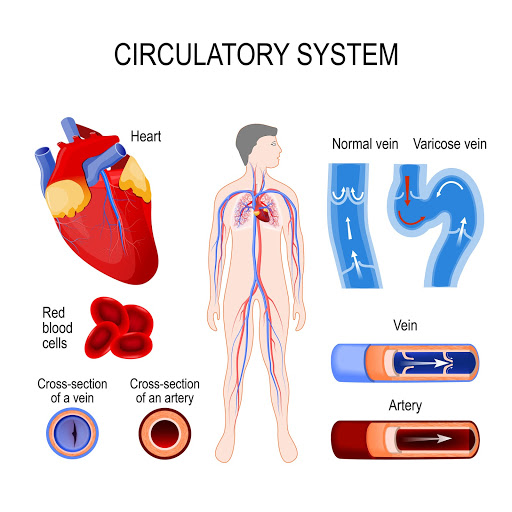
Venous insufficiency, also called venous reflux, is a debilitating leg issue in which the blood can’t flow up through the veins toward the heart. Healthy veins contain a number of specialized, one-way valves that open to allow blood to flow upward and close to prevent blood from flowing back down. When these valves are damaged or malfunctioning, venous insufficiency occurs.
As the valves deteriorate, the blood flows backwards and increases the pressure in the vein, dilating it. Blood stagnates, or pools, in the veins of the lower legs, putting pressure on the venous wall and causing inflammation and discomfort.
In many patients, untreated superficial venous reflux leads to the deposition of red blood cells in the tissues. Hemoglobin, the protein in red blood cells that carries oxygen, and hemosiderin, the accumulation of iron from the breakdown of hemoglobin , leaves deposits in the skin in the form of dark staining.
In severe cases, chronic, untreated venous insufficiency can cause open sores to develop on the skin, known as venous ulcers. These ulcers occur at the site where blood pools, due to the swelling that prevents the movement of nutrients and oxygen to the tissues.
Venous insufficiency can also cause varicose veins, a condition in which the superficial veins, or the veins closest to the surface of the leg, enlarge, twist, or bulge. In addition to being unsightly, varicose veins can cause pain, discomfort, or the development of venous ulcers.
If left untreated, venous ulcers can become infected, even gangrenous, leading to more risks or complications.
What Causes Venous Insufficiency and Venous Stasis Ulcers?
Venous insufficiency risk increases with age, but it can also be a result of genetic factors. If your family has a history of varicose veins, it’s more likely that you’ll also develop them. Those living either a sedentary lifestyle or spending long periods on their feet are also at risk of venous insufficiency.
Venous insufficiency can be caused by a partial blockage of the veins, such as a deep vein thrombosis (DVT), or blood clot.
Other risk factors include:
- Diabetes mellitus.
- Congestive heart failure.
- Peripheral vascular disease.
- Pregnancy.
- Obesity.
What Are the Symptoms of Venous Insufficiency and Venous Stasis Ulcers?
The most common symptom of the onset of venous insufficiency is chronic swollen ankles, feet or calves. The swelling is typically accompanied by cramping, dull aching or a feeling of heaviness in the legs, which worsens after prolonged periods of standing.
As venous insufficiency progresses, patients will experience skin discoloration with brown patches or flaking and hardening of the skin around the ankles. Left untreated, these can lead to venous ulcers.
Venous ulcers present with irregularly shaped, shallow wounds. Though they start small, they frequently expand to large wounds, typically around the lower leg on the medial or inside ankle. The base of the ulcer is usually red and may have exudate, or oozing of blood, depending on the level of infection. These wounds are often very painful. Frequently the entire leg will also swell, and the skin will take on a firm and reddish-brown appearance, known as stasis dermatitis.
Stasis dermatitis is another complication that’s common in individuals with poor venous circulation and often occurs in the lower legs, with or without ulcers. Like venous insufficiency, stasis dermatitis can cause swelling in the legs and feet, open sores and itchy, red skin.
It’s believed that stasis dermatitis is the result of a protein called fibrinogen, which leaks into the tissues and is converted into an active protein, fibrin. Fibrin then surrounds the capillaries in what is known as fibrin cuffs. This damages the tissues by preventing oxygen from entering.
Left untreated, stasis dermatitis can cause:
- Chronic venous ulcers.
- Osteomyelitis, a bone infection that can lead to septic arthritis, impaired bone growth, bone death or skin cancer.
- Osteomyelitis that may lead to amputation.
- Bacterial skin infections, such as abscesses or cellulitis.
- Permanent scarring of the affected areas.
Stasis dermatitis has the same risk factors as venous insufficiency. In fact, stasis dermatitis is a result or complication of prolonged venous insufficiency. it can be prevented by treating the symptoms of venous insufficiency before stasis dermatitis can cause ulcers.
Preventing Venous Insufficiency and Venous Ulcers

Fortunately, venous insufficiency and venous ulcers, along with their complications, can be prevented through a number of lifestyle changes.
Cigarette smoke is a vascular constrictor, which means it tightens the veins and arteries in the body. As a result, smokers are more likely to experience circulatory problems, so it’s important to quit smoking to prevent venous insufficiency from progressing.
Obesity is also a big risk factor in venous insufficiency. Reaching a healthy weight through diet and lifestyle changes is an effective way to reduce the pressure on the veins in the lower leg, which subsequently alleviates many of the symptoms of venous insufficiency.
Many underlying conditions have venous insufficiency as a potential complication. Individuals with high blood pressure or diabetes are more likely to develop venous insufficiency and venous ulcers, so efforts should be made to correct these conditions with the help of a physician.
Regular exercise promotes healthy circulation and reduces swelling in the lower legs. Individuals with a sedentary lifestyle are more likely to experience circulatory problems and venous insufficiency, so it’s important to have an active lifestyle. This could be as simple as short walks, light jogs or riding a stationary bike a few times a week. Mild stretching also helps to improve blood flow in the legs.
Tight clothing and shoes can restrict blood flow in the legs and increase the risks of chronic venous insufficiency. Individuals at risk for venous insufficiency should wear loose-fitting clothing and well-fitting shoes, avoiding high heels altogether.
Salt or sodium in food can contribute to water retention, which worsens the swelling in the legs and puts pressure on leg veins. Over time, this weakens the venous walls and may lead to insufficiency. Individuals at risk for insufficiency should lower salt intake and monitor sodium in processed foods to keep blood pressure levels healthy and reduce swelling.
Combined, these lifestyle changes promote healthy blood pressure levels and circulation, as well as helping to maintain a healthy weight, all of which work to reduce the risk of venous insufficiency.
Diagnostic Testing

In addition to a thorough medical history and physical examination to evaluate risk factors, diagnostic testing for venous insufficiency and and the development of future venous stasis ulcers may include:
- Duplex ultrasound: This is a vascular ultrasound procedure done to evaluate the blood flow and condition of the venous walls. Two types of ultrasound are used, a doppler and B-mode. The B-mode transducer obtains an image of the vessel, while the doppler probe evaluates the direction and speed of the blood flow within the vessel.
- Magnetic resonance venography (MRV): This is a procedure that uses a combination of a large magnet and radio frequencies to produce detailed imagery of structures and organs. It uses intravenous contrast dye, which gives the blood vessels an opaque appearance, to get a holistic view of the venous system,.
- Ankle-brachial index: This is a noninvasive test that’s used to check for peripheral artery disease, which is the narrowing of blood vessels that reduce blood flow. This test compares the blood pressure in the ankles with that of the arm to isolate and evaluate the blood flow in the legs.
 Treatment Options
Treatment Options
Venous Insufficiency and Varicose Veins
Treatment for chronic venous insufficiency depends on many factors, including:
- Specific symptoms.
- Age.
- Severity of condition.
- Tolerance for medication or procedures.
Many noninvasive treatment options are available for venous insufficiency, all of which aim to reduce the swelling and improve the blood flow to the heart. These include:
- Elevating the leg above the heart, which helps the blood flow away from the foot and toward the heart, decreases the blood stasis and, by extension, decreases swelling.
- Exercise, which stimulates the muscle movement and circulation in the legs to restore normal blood flow.
- Compression stockings, which are specialized medical devices that apply pressure to the leg and ankle to improve blood flow and reduce swelling.
Medication is also among the options for treating venous insufficiency, including:
- Diuretics: These are medications that draw fluid from the body and excrete it through the kidneys to reduce edema.
- Anticoagulants: These are medications that thin the blood, reducing the potential for blood clots and pooling.
- Pentoxifylline: This is a medication that improves blood flow.
Surgical treatment options for venous insufficiency or varicose veins include:
- Surgical repair of the veins or valves. This is not typically feasible.
- Removing the damaged vein. Vein stripping or phlebectomy.
- Minimally invasive endoscopic surgery, which involves the insertion of a thin tube with a camera to locate and seal varicose veins. This is mainly theoretical and Not common.
- Vein bypass, which is a procedure that transplants a healthy vein from another area of the body to the affected vein. This is typically used for the upper thigh, and only in severe cases–often of the deep vein system. .
- Vein ablation:a procedure that destroys or closes off the source of reflux,damaged vein.This typically involves a catheter placed within the vein.
- Radiofrequency ablation converts radiofrequency waves to heat
- Endoscopic venous laser therapy uses laser to heat the blood
- Venaseal uses a gluelike substance to occlude the vein.
- Varithena uses a Microfoam of chemical and oxygen to ablate the source vein.
- Ambulatory phlebectomy, which is an outpatient procedure that involves local anesthetic for specific areas of the leg before removing smaller varicose veins.
- Sclerotherapy, which involves a chemical injected into the damaged vein to restrict blood flow. This allows the blood to travel through healthy veins, and eventually the damaged vein will be absorbed. Sclerotherapy is only used in severe cases on small to medium-sized veins.
Venous Stasis Ulcers

Ulcers are easier to prevent than treat, especially when venous insufficiency is identified and treated early. Once they develop, several treatment options exist:
- Topical creams: In some cases, a topical cream with hydrocortisone can be used to minimize itching. Anti-fungal creams may also be used to prevent the development or spread of infection onto the feet or toes. In most cases, however, antibiotic creams may worsen inflammation and are avoided.
- Compression stockings: In addition to treating the underlying venous insufficiency, compression stockings may also be used to facilitate circulation and prevent backwards blood flow, reducing the swelling near the ulcer site. Compression stockings may also prevent venous ulcers from worsening and promote healing of existing ulcers.
- Unna boots: An Unna boot is a moist gauze bandage that is used on the lower leg from the area of the ulcer to below the knee. The gauze hardens to create a firm, tight boot around the leg. This support improved blood flow in the veins and facilitates healing of the ulcer.
- Transparent dressing: A transparent dressing is a clear, plastic-like film that is applied directly to a wound. A support stocking is usually placed over the dressing to improve circulation.
- Hydrocolloid dressing: A hydrocolloid dressing is a specialized bandage with a breathable layer that prevents liquid and pathogens from accessing the wound, while the inner layer absorbs exudate from the wound to promote healing.
Surgical options for venous stasis ulcers include:
- Debridement: Debridement involves the surgical removal of all non-viable, infected tissue and bone from an ulcer that isn’t healing properly. This process activates the platelets and growth factors to promote healing. This is often done if there are signs of infection, such as an elevated white blood cell count, fever and increased drainage of the ulcer.
- Laser treatment: Laser treatment may be used for chronic venous insufficiency if the veins in the leg should be closed to reduce pressure at the site of the venous ulcers. This procedure involves the insertion of a tiny fiber into the vein through a catheter, which uses a laser to destroy the diseased portion of the vein.
- Closure ablation: Ablation involves the insertion of a thin, flexible catheter that heats the venous walls with radiofrequency energy to destroy the vein tissue. This renders the vein incapable of carrying blood, leaving it to be absorbed by the body.
Vein Treatments at Vegas Valley Vein Institute

At Vegas Valley Vein Institute, we offer a full service vein evaluation and treatment. Vegas VAlley Vein utilizes numerous technologies and procedures to address venous insufficiency and prevent the future development of venous stasis ulcers.
Venefit – Radiofrequency Endovenous Ablation
The Venefit (VNUS Closure) Procedure is a non-surgical alternative for treating varicose veins. This uses radiofrequency (RFA) energy to heat and contract the collagen within the venous walls, causing them to collapse and seal. Radiofrequency endovenous ablation is a minimally invasive ambulatory treatment alternative to the surgical stripping of a vein. It addresses the underlying cause of varicose veins, making it a highly effective treatment for venous reflux disease. Once closed, the blood then travels through healthy veins.
Venefit is an outpatient procedure with minimal downtime, with many patients returning to work the same day and to normal activity within one to two days. Venefit provides long-lasting relief of symptoms and leaves little to no scarring.
VENASEAL
The VENASEAL procedure closes the problematic veins by occluding them with a methylmethacrylate glue like substance. By closing off the problematic veins, blood is then forced to route through healthier working veins that do not have valve problems and reflux.
VARITHENA
VARITHENA Microfoam Chemical ABlation is a chemical foam made with polidocanol and oxygen. The foam is injected through an IV or small butterfly needle. It is observed owith Ultrasound and allowed to flow through even the large and tortuous veins. It can be stopped by simple pressure and as the oxygen is absorbed across the vein lining, the medication is left on the vein wall to cause a chemical ablation or destruction of the targeted problematic veins.
Asclera
Asclera is a sclerosing agent that’s injected into the vein and damages the endothelium, or the cells that line the wall of the vein. This causes blood platelets to attach to the lining, causing it to clot over time. The clotted vein is eventually replaced with scar tissue.
Asclera is a fast, minimally invasive procedure that leaves no scars and provides immediate relief of symptoms. The results are long-lasting as well. Unlike Varithena, Asclera is really only of value in treating spider veins and small reticular veins. We often utilize Asclera to complete a patient’s leg vein treatments–clearing unsightly spider and reticular veins after one or more other modalities above have been utilized to treat the underlying larger veins that are the source of the problem.
Ambulatory Phlebectomy
An ambulatory phlebectomy is a method of removing varicose veins on the surface of the legs. This procedure is performed under local anesthesia and involves small punctures or incisions to remove the varicose veins.
Because an ambulatory phlebectomy is done with local anesthetic, there’s minimal recovery time and patients return to normal activity in one to two days. It also provides long-lasting results and minimal scarring.
Visit Vegas Valley Vein Institute
If you suffer from varicose veins, or other symptoms of venous insufficiency, Vegas Valley Vein Institute can help. We’ll work with you to evaluate the severity of your condition and determine the best treatment option(s) for your unique needs. We offer many minimally invasive treatment options to treat varicose veins and prevent the complications that come from venous insufficiency. Contact us today to schedule your consultation!
